Nature-based social prescribing for mental health
The Therapeutic Nature project was led by Dr Ruth Garside and was a collaboration between researchers at ECEHH, University of Exeter, PenCLAHRC, University of Plymouth and Exeter, NHS Born in Bradford and eftec.
The report is aimed primarily at governmental (national and local) departments or bodies with responsibility for, or an interest in the development and use of NBSP. It may also be relevant to those organisations and individuals involved in the development and delivery of NBSP. The report informed the development of the Government’s Green Social Prescribing Test and Learn Pilots. The new work is closely aligned with the MRC funded Nature on Prescription project which has led to the production of a Nature on Prescription Handbook
The final report, and research briefing, Therapeutic Nature: Nature-based social prescribing for diagnosed mental health conditions in the UK project has now been published. The 12 month project aimed to identify what works in the use of nature-based therapeutic interventions for people with an identifiable mental illness.
One of the key aims of the Government’s 25 Year Environment Plan is to help identify how we can best use the natural environment as a resource for preventative and therapeutic health programmes. This research will help improve understanding of active elements of therapeutic nature interventions and will clarify how they can be planned, delivered and embedded in wider practice.
There were four key strands to the 12 month project:
Work Stream 1: Review and map current provision of nature-based therapeutic interventions, including commissioned and non-commissioned services and schemes, to support people with a mental illness. The aim was to understand: which population groups are participating; types of interventions and their nature; funding models; costs; relationship with health and social care organisations.
Work Stream 2: Review the current available evidence base for the effectiveness of therapeutic nature-based interventions. We used rapid systematic review approaches to assemble and synthesise existing evidence for the therapeutic effects of nature-based interventions. The work aimed to identify the mechanisms through which interventions may impact on core mental health symptoms and behaviours; which outcomes are likely to be appropriate measures of impact and the factors that facilitate or hinder intervention implementation and adherence, including medical, governance and financial factors.
Work stream 3: Gather insights from key stakeholders to understand perceptions about what works, and the factors that influence success in commissioning, delivery, and implementation. The team sought to include service commissioners, mental health service professionals, primary health care services, environmental voluntary organisations, community-based providers and other intermediaries in the four key locations.
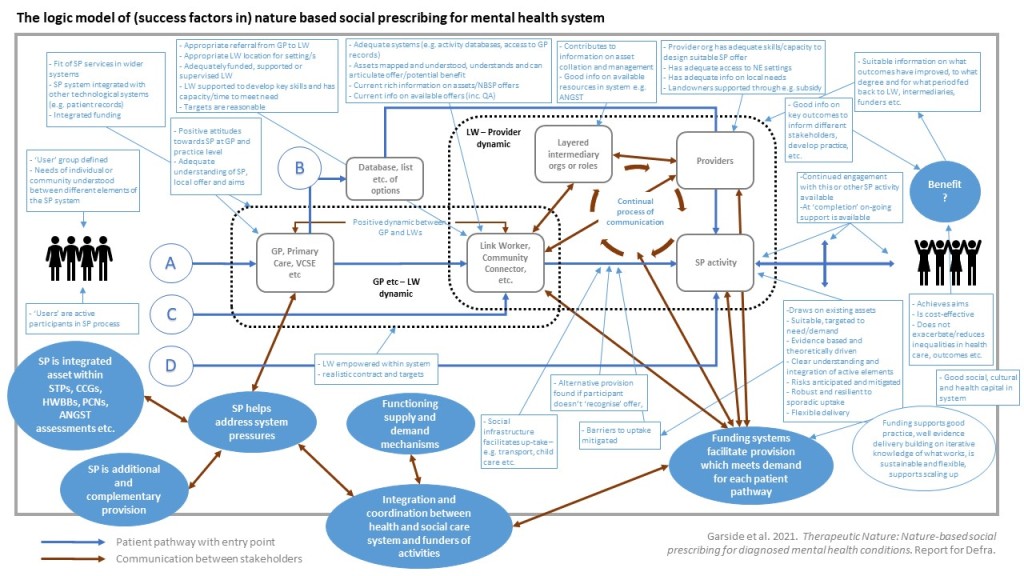
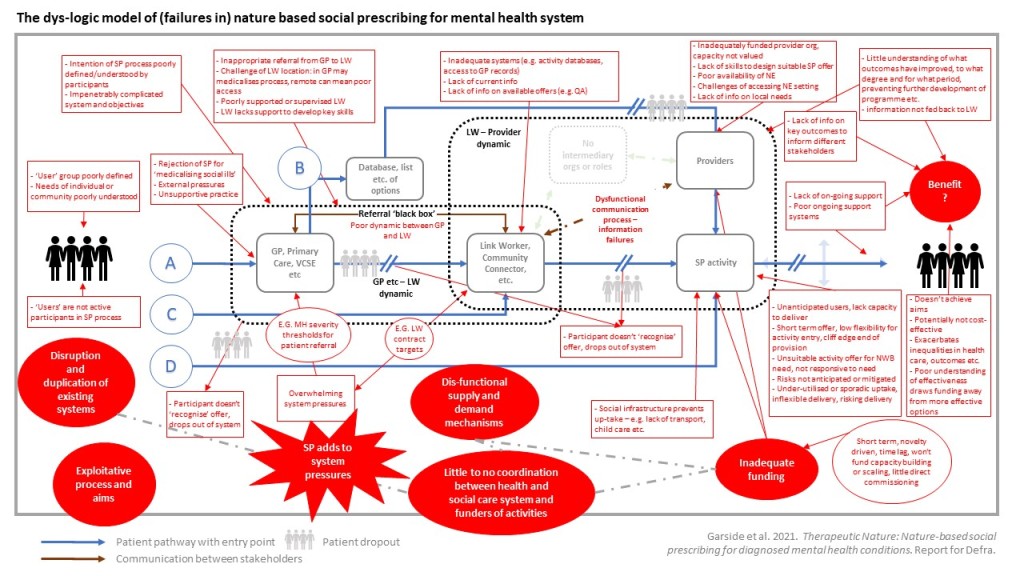
Work stream 4: Synthesis, The team brought together insights from the mapping, evidence review and qualitative insight work to produce a detailed conceptual framework, descriptive texts and illustrative case cases. The work focused on understanding and explaining the factors that affect successful provision of nature-based therapeutic interventions for people with mental ill-health and how these may be mitigated against. This included understanding key elements of the social prescribing system where challenges may occur and how these barriers may be overcome, as well as describing successful approaches at each step. We also identified opportunities to build on existing provision, together with understandings of what works, for whom, in what circumstances. This provided opportunities to propose how new, larger scale, sustainable and more systematic approaches to offering and delivering nature-based mental health therapies may be developed.
Key findings
- There is a significant amount of nature-based activities offered by mental health and environmental NGOs, social enterprises, community interest companies (CICs), local councils, NHS trusts, and private therapists. However, there is wide variability of the nature and scope of these offers, within and between districts. Often projects are collaborative between multiple organizations. Referral bodies include primary care, mental health services, social care and educational institutions, people may also self-refer.
- Many social prescribing activities are targeted at adults experiencing social isolation, loneliness and anxiety with complex needs. While some nature-based social prescribing (NBSP) activities are designed as therapeutic, and others promote resilience, or provide enjoyable experiences, others are rather unspecific about which participants they are targeting. Some activities include therapeutic aspects such as formal counselling or therapy, other intervention components, such as skills learning or creative activities, may also be used.
- Current capacity within the system is challenging to understand. There is poor coordination of demand and supply at a national or local level.
- Most NBSP offers are short term (~12 weeks), supported by project funding from bodies such as Big Lottery. There was some evidence of commissioned models, these tend to be pilots. There is a reliance on 3rd party funders whose goals sometimes align with national level priorities of the health system (e.g. the focus on better mental health) but not necessarily with local needs.
- There are positive perceptions towards NBSP activities offered through social prescribing across the system, however this is not universal.
- The mechanisms through which information is shared on individual NBSP specifics with the referral body is often patchy, ad hoc and, in some cases, insufficient to allow the link worker to make informed decisions about referrals. Stakeholders struggle to maintain sufficient information. In the referral system this information deficit relates to the availability and specifics of NBSP activities, in the delivery system this information deficit relates to health and care system needs, engagement routes, and evidence standards.
- There is little robust quantitative research evidence for the effectiveness of nature-based social prescribing, however, we found some evidence that nature-based activities can positively impact on depression, anxiety, mood and feelings of hope. Higher quality qualitative evidence revealed how the activities are experienced and perceived to benefit.
- We identified a number of key elements which need to be in place for NBSP to be effective: coordination of NBSP within wider systems of health; where NBSP is additional and complementary to other services; if appropriate and informed referrals are made; where there is adequate information sharing between stakeholders; there is clarity in the aims and process of the NBSP; where NBSP activities are evidence based and theoretically driven; and provider organisations have adequate skills and capacity to design and deliver suitable NBSP offer.
Recommendations
The report identified a number of key recommendations for further developing and NBSP, these include: 1) advocacy for NBSP across systems; 2) identifying mechanisms to facilitate coordination of supply and demand in NBSP at a strategic level; 3) enhancing knowledge sharing, peer support and advocacy through a network and one-stop shop for nature-based social prescribing; 4) enhancing capacity of local coordinating bodies; 5) improving the funding system; 6) supporting the development of skills in nature-based social prescribing; 7) enhancing the usability of information on nature-based social prescribing; and 8) improving understanding of what works, how and for whom.
The Therapeutic Nature: Nature-based social prescribing for diagnosed mental health conditions in the UK report and briefing are published by Defra (Defra Project Code BE0155) and are available from the Department’s Science and Research Projects Database at http://randd.defra.gov.uk. Whilst the research was commissioned and funded by Defra, the views expressed reflect the research findings and the authors’ interpretation; they do not necessarily reflect Defra policy. ab
It builds on the findings of an earlier systematic reviews, as well as this Attention Restoration Theory Review